In our four-part series on specialty drug management, we have covered the importance of monitoring drugs before FDA approval and determining formulary placement, as well as proper utilization management strategy. Now we’re going to discuss how to plan for the financial impact of a new specialty medication.
The strategies we’ve already employed with formulary placement and utilization management ensure that it’s the right drug for the right member at the right time and dose; however, with these medications costing an average of $5,000 per claim, plan sponsors need to prepare for how this will impact their budget.[1] Emerging new therapies focus on addressing the needs of rare, orphan or even genetic-related conditions. With the population being extremely small and drug costs typically extremely high, these therapies can have a profound financial impact on a member and plan, hitting both the prescription and medical benefit. Budget impact modeling can help a plan prepare for these circumstances.
 Preparing for Pipeline Updates
Preparing for Pipeline Updates
In order to properly prepare for new specialty medications, it’s important to keep an eye on the development pipeline. As mentioned in our first article in this series, Elixir’s team of clinical pharmacists monitors and reviews drugs prior to FDA approval, tracking numerous pharmaceutical agents throughout the research and development process. We share information on pipeline developments with our clients in our Weekly Drug Update emails, including notable drugs in the research phase, recent FDA approvals, and new generics and indications. This insight allows clients to begin preparing before a drug is approved.
Predicting the Impact
Elixir has the ability to provide our clients with an in-depth predictive view of a drug and its potential impact based on the membership details, whether it’s a new specialty drug to market, a new or expanded indication for an existing medication, or a generic or biosimilar becoming available. The analysis takes into account the client type (i.e., Medicare, Medicaid or commercial) and size. With this data, we compare the new or updated drug to existing medications that are approved to treat the same condition, summarizing the potential cost impact over time, whether it be additional spend or savings.
With this insightful tool, we can provide clients with predictions on the following:
- Number of members who might utilize a particular drug
- Expected cost of a new drug
- Impact of a generic drug entering the market
- Per member per month (PMPM) costs
- Cost shifts when additional treatments are approved
In addition, we can share with clients what diagnosis codes to look for within medical claims to determine if a member has a rare condition that a new orphan drug treats in order to more accurately predict the financial impact of that therapy.
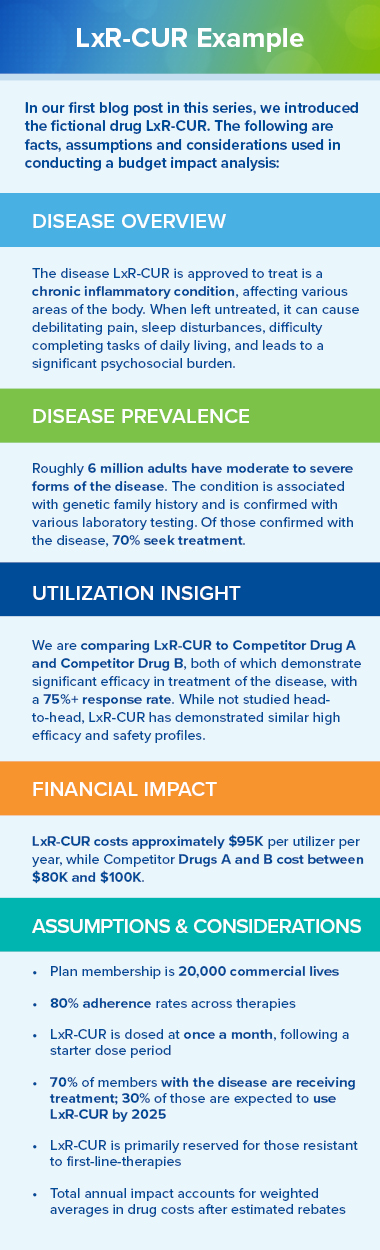
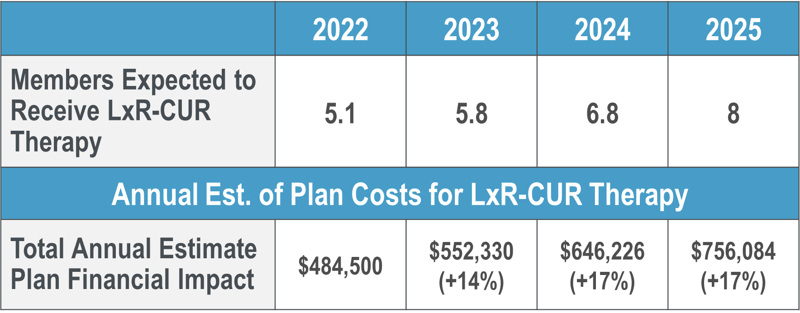
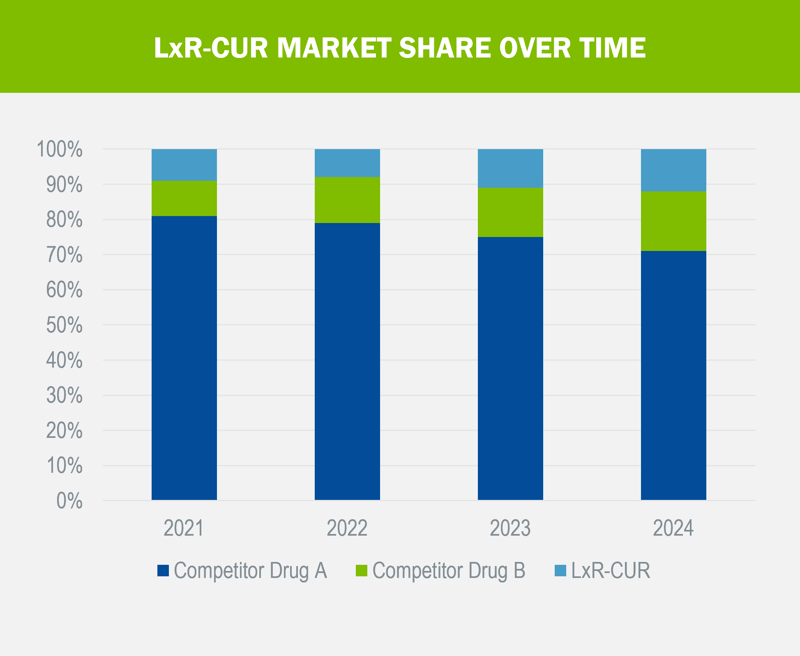
Let’s take for example our fictional drug, LxR-CUR, that we’ve been following throughout our series. LxR-CUR is a specialty medication that was just approved in January of this year to treat an inflammatory condition that affects approximately 6 million adults, with around 70% of those diagnosed seeking treatment. For our analysis, we compared it with two different medications already on the market, Competitor Drug A, approved in March 2017, and Competitor Drug B, approved in September 2020. Both medications have demonstrated significant efficacy in treatment of the disease, with a 75%+ response rate and cost between $80K and $100K per utilizer per year (PUPY). While LxR-CUR was not studied head-to-head against these medications, it has demonstrated similar high efficacy and safety profiles at a cost of $95K PUPY. Following are the results of the analysis for a 20K-life commercial plan:

Proactive Preparedness
While there’s sometimes only so much you can control when a member starts taking a pricey new specialty medication, particularly when there are not other options to treat a serious condition, Elixir’s budget impacting tools allow our plans to proactively prepare for new therapies to market using data, trends and facts so it’s not like receiving a sucker punch to the budget. This information can be empowering and ease anxieties, allowing plans to make informed decisions about plan design, budget accordingly and put measures in place to create cost efficiencies, all while ensuring the member has access to potentially life-saving medications.
In the final part of our series, we will discuss how a specialty pharmacy can ensure both the member and the plan get the most out of costly treatments.
[[1] U.S. Pharmacist (2021). Net Spending on Specialty Pharmaceuticals Surging. https://www.uspharmacist.com/article/net-spending-on-specialty-pharmaceuticals-surging.

