Hundreds of prescription medications process every day and patients and plan sponsors pay for them because that's what they are supposed to do, right? Maybe, maybe not. Are there some medications hiding in your claims that just shouldn't be there at all? Are there seemingly normal looking prescriptions that are priced much higher than alternatives? Are there medications that aren't FDA approved? It's time to unmask these sneaky medications and control them before they can negatively impact your drug spend.
Let’s start by explaining a couple types of these medications and why they can be an issue for plan sponsors.
New but not necessarily better
There is an emerging trend in which pharmaceutical companies combine already-approved, lower-cost medications to create a new, brand prescription medication. This tactic extends the life of the medications’ patent protections, and, in the end, the “new” medication gets a new name and often a new high cost.
While these medications may be safe and effective, they provide no clinical advantage or health benefit over the lower-cost alternatives already on the market. In fact, the active ingredients between the old and new medications are nearly identical.
For example, the brand medication Treximet®, used for acute treatment of migraine attacks, is the combination of generic medications sumatriptan and naproxen. If we break this down, naproxen is available over the counter as Aleve®. If a patient gets a prescription for the generic sumatriptan and then buys the over-the-counter Aleve, this treatment will contain the same ingredients as the brand medication Treximet. The patient will be taking two tablets instead of one, but the big difference is in the price. The monthly cost for Treximet is $900. (That in itself might cause a headache.) The monthly cost of the sumatriptan plus the Aleve is just $34.
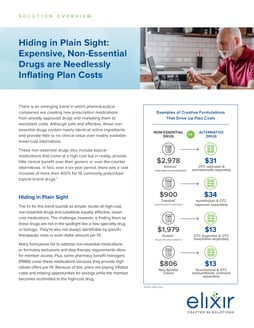
These new medications are simply not essential and all they deliver is an unnecessarily inflated drug spend for plan sponsors and members. Along with Treximet, the following table highlights the active ingredients similarities and the huge disparity in prices for a couple of other brand drugs versus their lower-cost alternatives.
|
NEW BRAND MEDICATION |
PRICE |
ALTERNATIVE |
PRICE |
|
Treximet (sumatriptan/naproxen) |
$900 |
sumatriptan and OTC naproxen |
$34 |
|
Vimovo® (naproxen-esomeprazole) |
$2,978 |
OTC naproxen & esomeprazole separately |
$31 |
|
Duexis® (ibuprofen/famotidine) |
$1,979 |
OTC ibuprofen & OTC famotidine separately |
$13 |
While formularies are a great tool for managing unnecessary drug spend, these drugs are not easy to find, and payers aren’t actively looking for them. These medications slide into a claim unnoticed as they:
- Don’t typically fall into a specific therapeutic class or even dollar amount per fill.
- Are not usually in the spotlight, like a specialty drug or biologic.
- Don’t set off any alarms and, in many cases, the manufacturers are advertising their medications to doctors and directly to consumers, often offering coupons and discounts to encourage use.
Not reviewed or approved
Another trend is with drugs that have not been reviewed by the U.S. Food & Drug Administration (FDA) for safety, effectiveness or quality, yet they are slipping into the pharmacy benefit. The FDA review is required by law for all new medications, and, without it, there is no way to know if these drugs are safe and effective for their intended use, whether they are manufactured in a way that ensures consistent drug quality or whether their label is complete and accurate.[1]
The non-FDA-approved medications may still have national drug codes (NDCs), which populate in a drug database like Medi-Span. Because of this, claims for these medications may process just like an FDA-approved medication without the healthcare professional or member knowing of the unapproved status. The non-FDA approved medications hide in plain sight within claims without any warning and their use could cause a patient undue harm.[1]
Sometimes, non-FDA approved drugs process as 510(k) medical devices, often with extremely high price points. For example, a topical “prescription only” agent for atopic dermatitis or eczema that is just a moisturizer is marketed as a medical device and sneaks into coverage under the pharmacy benefit at a cost of over $5,000 per script.
The FDA does permit some unapproved prescription drugs to be marketed if:[1]
- The drug is subject to an open drug efficacy study implementation (DESI) program proceeding.
- Healthcare professionals rely on the drug to treat serious medical conditions when there is no FDA-approved drug to treat the condition.
- There is insufficient supply of an FDA-approved drug.
Discover the troublesome medications hiding in plain sight
These non-essential and non-FDA approved medications are processing through your claims right now, completely unnoticed, driving up costs and risks. Short of evaluating every single prescription presented to identify the culprits, your plans need a program that can stop these medications from processing, save on drug costs and provide clinically sound medication alternatives for your members.
Work with a pharmacy benefit manager (PBM) to initiate a clinical strategy to mitigate the risk and costs of
non-essential and non-FDA approved medications. With the right program in place, members will get safe medications at more affordable prices and payers will have an effective tool to better control unnecessary drug spend.
References
- Unapproved Drugs, 06/02/2021, U.S. Food & Drug Administration, https://www.fda.gov/drugs/enforcement-activities-fda/unapproved-drugs, Accessed May 25, 2023