Even before the COVID-19 pandemic made its mark on history, large numbers of consumers were increasingly demanding access to information on their terms—whenever, wherever and however they wanted. These “always-on” consumers, as they’ve been called, make up about 44% of Americans in the 18- to 49-year-old range and an additional 30% of those aged 50 and older.[1] As a result of their constant access to information and services, consumers have begun learning more about their health and playing a more active role in their care.[2]
Unfortunately, despite greater information and engagement, more than 50% of consumers still have low healthcare literacy, meaning they don’t understand common terminology, such as “premiums,” “deductibles” and “coinsurance” nor do they understand networks, prior authorizations and other coverage concepts. This lack of healthcare literacy is frustrating for consumers and can mean they don’t always end up making the best decisions for their care.[3]
At Elixir, we understand that consumers want greater control of their healthcare while needing better guidance with navigating the system, so we’ve been enhancing our member experience, including virtual benefit fairs, easy-to-understand welcome kits, an integrated member portal and mobile app, and an upgraded call center. With these tools, members can learn more about managing their health and more easily understand their coverage.
A New Approach to Benefit Fairs
To help members understand their pharmacy benefit options, we often host benefit fairs for clients. Starting in 2020, with the COVID-19 pandemic limiting in-person contact, we shifted our benefit fairs online, making pharmacy benefit information accessible to members in the safest way possible.
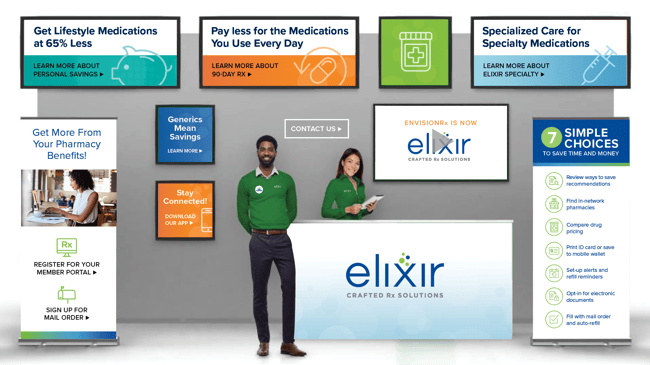
Our virtual benefit fairs (VBFs) are very much like in-person events, where members can collect informational flyers, watch videos and contact us for more information. The added bonus of a VBF is that members can access their unique online benefit fair securely at their own convenience—any time of the day or night.
Even as in-person events begin to occur again, we’re planning to keep VBFs as ongoing options. New enhancements coming soon include client-customized materials, a tour of our pharmacy, and integrated surveys for members to share their feedback and help us continue to improve this offering.
Uncomplicating Pharmacy Benefits for Members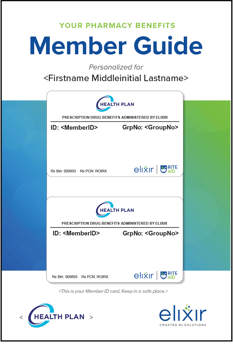
To help members better understand their benefits and navigate their prescription drug coverage, we’ve developed a more comprehensive welcome kit and formatted it as a handy digest-sized booklet that is easy to read and understand.
In the booklets, we explain commonly used terms and provide information on simple choices members can make to improve their health. We’ve also put the Member ID cards on the front of the booklets, where members can easily find them, which has dramatically reduced requests for duplicate cards.
Additionally, the booklets clearly instruct members about how to access their online accounts and the mobile app, where they can more easily manage their medications and monitor their coverage 24/7 using a computer or mobile device.
With these enhancements, the new member kits are proving to be a helpful tool for members to educate themselves and stay informed on their coverage.
On-the-Go Access 24/7
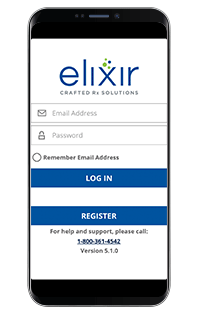 With our member portal and mobile app, members can easily access all of their pharmacy benefit information in one convenient location, anytime, anywhere. Earlier this year, we debuted an all-new, more integrated member portal and mobile app, providing an even more user-friendly experience, so members can easily have all their pharmacy benefit information available at their fingertips in one convenient location, whether they’re at home or on the go.
With our member portal and mobile app, members can easily access all of their pharmacy benefit information in one convenient location, anytime, anywhere. Earlier this year, we debuted an all-new, more integrated member portal and mobile app, providing an even more user-friendly experience, so members can easily have all their pharmacy benefit information available at their fingertips in one convenient location, whether they’re at home or on the go.
Now, when members are in their doctor’s office or at the pharmacy, they can quickly and easily:
- Access their Member ID card information digitally to confirm coverage
- Check if specific drugs are covered, compare pricing at various pharmacies and be alerted to lower-priced alternatives before the prescription is even written
- Find pharmacies based on their specific needs and services, such as drive-through windows, extended service hours, immunizations and more
These tools also help members learn more about their health conditions and their medications, including cautions and possible side effects. Members can see their prescription order history, check refill availability and, if the plan uses Elixir Mail Order pharmacy, request refills online.
The recent improvements are just the beginning. We have more enhancements planned, with the goal of making the member portal and mobile app easier to use and making coverage easier to understand.
Help is Just a Phone Call Away
To round out our efforts to help members navigate their prescription benefit coverage, we offer a 24-hour call center staffed by U.S.-based representatives who have received extensive training on more than 50 topics. This includes general knowledge about insurance—so they can explain deductibles, copays and all the other terms—as well as how to use the online tools, resolve rejections, help members get direct reimbursements and much more.
While the complex healthcare system is likely to continue to pose challenges, our goal is that Elixir’s prescription drug benefits not be among those challenges. Instead, by focusing on members’ needs and making information available at their fingertips, we’re working toward ensuring that members have what they need to make the best decisions for their care.
[1] Perrin, A and Atske, S. (2021) About Three-in-Ten U.S. Adults Say They are ‘Almost Constantly’ Online; Pew Research Center; https://www.pewresearch.org/fact-tank/2021/03/26/about-three-in-ten-u-s-adults-say-they-are-almost-constantly-online/
[2] Betts, Korenda and Giuliani (2020) Are Consumers Already Living the Future of Health?; Deloitte Insights; https://www2.deloitte.com/us/en/insights/industry/health-care/consumer-health-trends.html
[3] Meltzer, R. (2018) More than Half of Consumers Don't Understand Basic Aspects of the Healthcare System, Survey Finds; Fierce Healthcare, September 2018; https://www.fiercehealthcare.com/payer/more-than-half-consumers-don-t-understand-basic-aspects-healthcare-system-survey-finds#:~:text=Payer-,More%20than%20half%20of%20consumers%20don't%20understand%20basic%20aspects,the%20healthcare%20system%2C%20survey%20finds&text=Contrary%20to%20what%20one%20might,a%20college%20or%20graduate%20degree

