Specialty medications continue to be a predominant topic in the healthcare industry, as more and more of these novel drugs are developed. In 2020, nearly 40 of the 50+ medications approved by the Food and Drug Administration (FDA) were specialty drugs.[1, 2] Even though only about 2% of Americans use specialty medications, they account for half of all drug spend.[3]
Like traditional medications, some specialty drugs have a generic alternative that costs a fraction of the branded original. Generics have long been seen as lower cost and therapeutically equivalent alternatives to traditional branded medications and have widespread acceptance. However, generic specialty medications are still not as widely accepted, even though they offer the same value as their traditional counterparts.
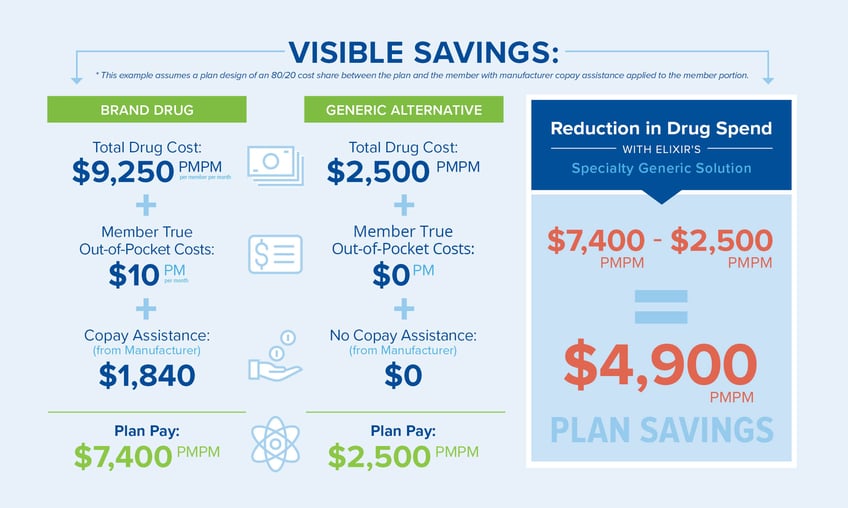
There are a variety of reasons for this lack of utilization, such as loyalty to brand name products, a perceived lack of efficacy, marketing influences and little-to-no incentives within benefit designs to encourage use. Additionally, with copay assistance routinely being offered by the branded drug manufacturers, members may be comfortable with the discount and not think about the actual cost. Yet, when members and prescribers choose to use generic specialty medications, the possible savings for both the plan sponsor and member are significant.
Elixir’s Specialty Generics solution encourages the use of generic specialty drugs. The solution uses a thoughtful approach to identify clinically effective generic specialty drugs with the greatest potential to positively impact plan sponsors by reducing drug spend. This helps protect payers and members against rising specialty drug costs by using generic alternatives when available.
With this solution, members get the benefit of a $0 copay when they fill these identified generic specialty medications, which is often less than the brand with the manufacturer assistance. The plan sponsor also benefits since the total amount they pay for the specialty generic—although it’s 100% of the drug cost—is significantly less than what they would pay for the branded drug, sometimes half the cost, resulting in thousands of dollars in reduced drug spend. Even if only a few members switch to the specialty generic medication, the decrease in specialty drug spend can be significant.
Elixir’s Specialty Generics solution provides an optimal way to impact the rising costs of specialty medications by incentivizing the use of clinically equivalent generic specialty medications, lowering spend for both the plan sponsor and member.
[1] Novel Drug Approvals for 2020, FDA. https://www.fda.gov/drugs/new-drugs-fda-cders-new-molecular-entities-and-new-therapeutic-biological-products/novel-drug-approvals-2020
[2] Rosenberg, Jaime. 2020 drug approvals: not bad, considering. Managed Healthcare Executive, December 16, 2020. https://www.managedhealthcareexecutive.com/view/2020-drug-approvals-not-bad-considering
[3] IQVIA Institute. Medicine Use and Spending in the U.S.: A Review of 2018 and Outlook to 2023. IQVIA website. https://www.iqvia.com/en/insights/the-iqvia-institute/reports/medicine-use-and-spending-in-the-us-a-review-of-2018-and-outlook-to-2023 Published May 9, 2019.


